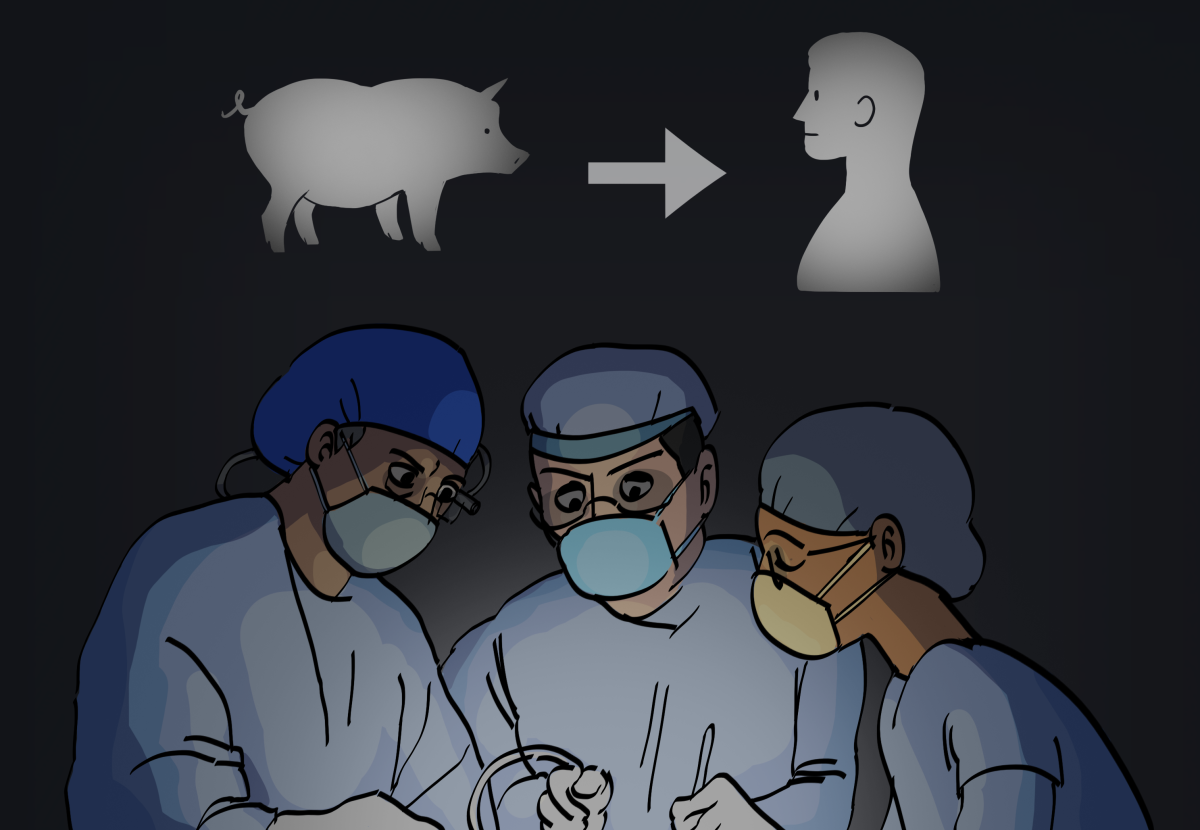
Although the idea of using an animal’s organ in a human transplant surgery may seem repulsive, it should be seen as a scientific victory especially because it can give someone the chance to keep living.
A recent surgery was done in September that resulted in a brain-dead person successfully being given a genetically modified pig’s kidney, according to an Oct. 19 New York Times article.
Before you shake your head and rule out the idea all together, this isn’t the first time animals have been used in medicine.
Cows and coincidentally pigs have been used to make insulin for years. In the U.S., manufacturing of beef insulin was discontinued in 1998 and pork insulin in 2006, according to an Oct. 28, 2015 Food and Drug Administration (FDA) Q&A on Importing Beef or Pork Insulin for Personal Use webpage.The discontinuation of animal-sourced insulins was a voluntary withdrawal of these products made by the manufacturers and not based on any FDA regulatory action, according to the same webpage.
Insulin in the U.S. is currently made from bacteria, with E. coli being the first genetically engineered bacteria to produce it, according to a July 1, 2019 American Diabetes Association article.
Insulin is a naturally occurring hormone secreted by the pancreas and is used to help the body utilize or store the blood sugar it receives from food, according to an American Diabetes Association’s Insulin & Other Injectables webpage.
While processing animals to make insulin isn’t an organ replacement, it serves as an organ function to help save lives.
In the U.S., there are more than 106,631 people waiting for an organ transplant. Almost 100,000 patients need kidneys and nearly 20,000 patients need a liver, according to a Health Resources & Service Administration Organ Donor Statistics webpage.
About 17 people die every day waiting for an organ transplant and every nine minutes another person will be added onto the transplant waiting list, according to the same webpage.
For this reason alone, genetically modified animal organs shouldn’t be disregarded and instead be used to help curb the demands of obtaining an organ.
In recent development of artificial organs, a nationwide research project, known as The Kidney Project, has successfully demonstrated a functional prototype artificial kidney, according to a Sept. 9 UCSF School of Pharmacy article.
The Kidney Project’s goal is to create a small, surgically implanted and free-standing bioartificial kidney to treat kidney failure, according to its website.
While the development of the artificial kidney prototype is hopeful to help supplement the growing demands of obtaining kidneys, there’s no timeline for when it will be released to the public.
The time to wait for artificial kidneys to come out may take too long given the lives at stake.
While the coronavirus is widely known to damage lungs, it can also damage kidneys.
More than 15% of hospitalized COVID-19 patients have acquired acute kidney injuries, in which many now require dialysis, according to a May 14, 2020 National Kidney Foundation article.
Dialysis is a treatment that removes wastes and extra fluid from a patient’s blood when their kidneys are no longer able to do so effectively, according to a National Kidney Foundation Dialysis webpage.
It would be foolish to disregard the use of genetically modified animal organs while the pandemic rages on and people continue to die.
The idea of using animal organs may freak people out but it shouldn’t be shunned. It has the potential to save the next patient in need of an organ, which could very well be you or someone you know someday.